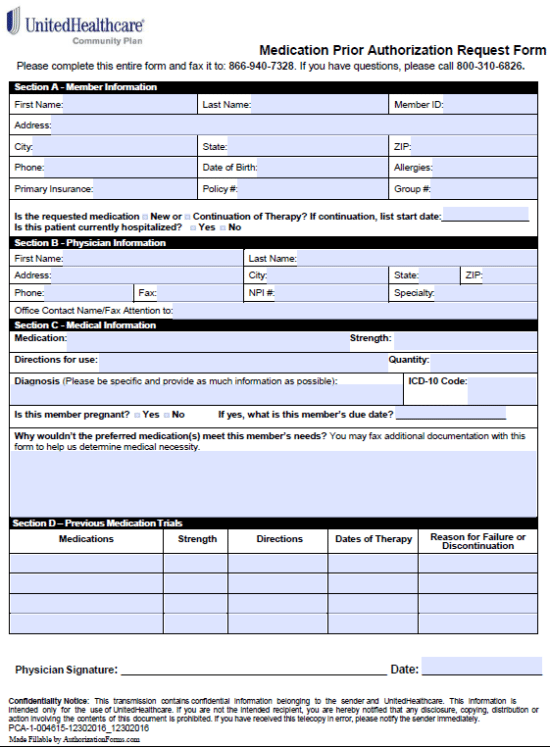
The United Healthcare Medication Prior Authorization Request Form allows a patient and United Healthcare beneficiary to request coverage for a medication that requires authorization, one that is generally not on the formulary. The prescriber/healthcare professional prescribing the drug will be required to justify their choice of the non-preferred medication in paragraph format on the document. If all sections are complete in full and the reasoning behind requesting the specialized drug is sound, United Healthcare will cover all or part of the price of the treatment.
State-specific forms:
How to Write
Step 1 – Begin by downloading the document in Adobe PDF.
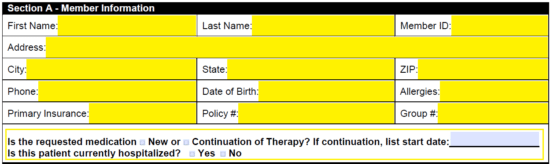
Step 2 – Beginning filling out the form on your computer or in black/blue ink. The first section will need the member information. This will require all of the following:
- Full name
- Member ID
- Address
- Phone number
- DOB
- Allergies
- Primary insurance
- Policy number
- Group number
At the bottom of this window, you will have to specify whether this is a new request or a continuation of a therapy. If it’s a continuation, provide the start date of the therapy initializing. Check “Yes” or “No” to indicate whether the patient is hospitalized.
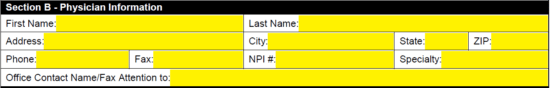
Step 3 – Physician information is next. Supply their full name, address, phone and fax number. Their NPI#, specialty must also be entered along with the name of the office contact.
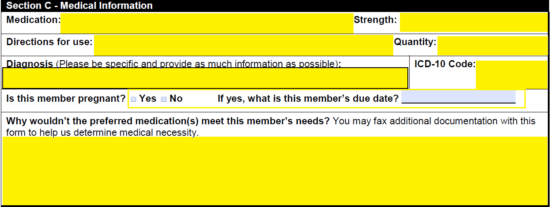
Step 4 – In “Section C” is where you’ll need to enter the medication’s specifications and give your reasoning and evidence for why the selection is medically necessary. Enter the following in the available fields:
- Medication
- Strength
- Directions for use
- Quantity
- Diagnosis
- ICD-10 Code
- If the member is pregnant and the due date (if applicable)
- Why you’re choosing this medication over one which is listed as “preferred”
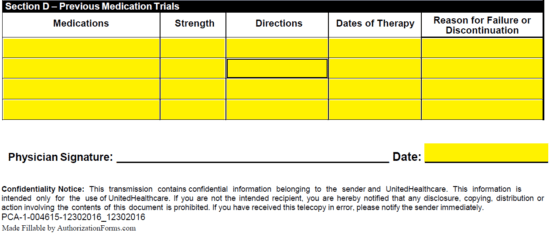
Step 5 – Previous medication trials must be submitted to help justify the request. Enter each medication, strength, directions, dates of therapy and reasons for failure in the table presented at the bottom of the form. Date the document and supply it with a signature before faxing it to: (866) 940-7328.