The Wellcare Prescription Drug Coverage Determination Form can be used for prior authorization requests, the demand by a healthcare practitioner that their patient receive coverage for a medication that they deem necessary to their recovery. It is usually necessary that previous therapies have been tried and failed in order for insurance companies to justify the prescribing of a more expensive, non-formulary drug. It is possible for prescriber, patient, and patient representative to make the request. All forms, once completed, should be faxed to 1 (866) 388-1767.
How to Write
Step 1 – Download the form in Adobe PDF.
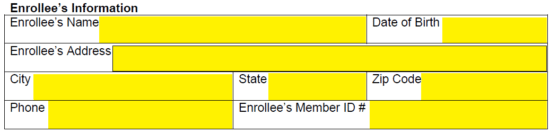
Step 2 – The enrollee’s name, DOB, address, phone number, and enrollee member number will need to be provided in the first section.
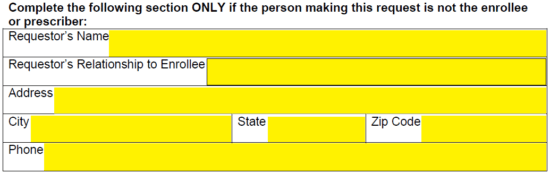
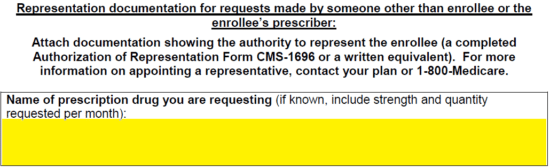
Step 3 – Next, submit the requestor’s name, relationship to enrollee, full address, and phone number. It should be noted that this is only applicable if the person making the request is not the enrollee or the prescriber.
Step 4 – Submit the name of the drug being request, as well as the strength and quantity request for each month (if possible).
Step 5 – In the “Type of Coverage Determination Request” window, select the prior authorization option.
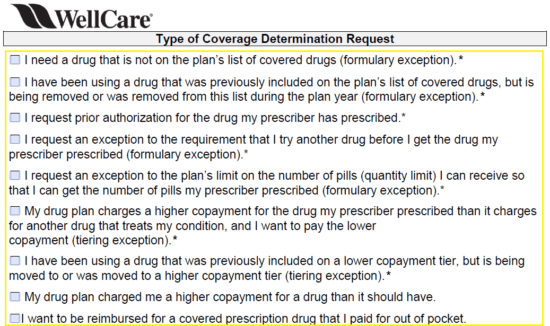
Step 6 – Any additional information that should be considered by Wellcare can be submitted in the available fields here or attached with supporting documents. If a decision is needed within 24 hours, check the applicable box. Provide the date and, when printed, your signature.
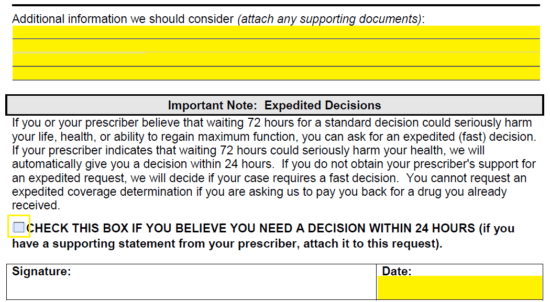
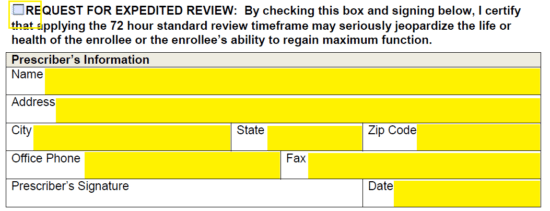
Step 7 – Again, if you need the form expedited, check the box on this page. Next, enter the prescriber’s info. The following will be necessary:
- Name
- Address
- Office phone
- Office fax
- Signature (once printed)
- Date
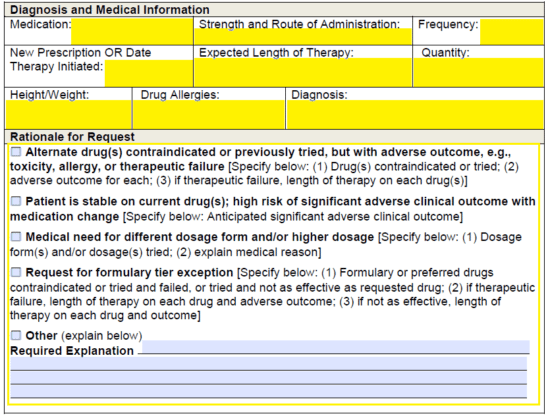
Step 8 – The “Diagnosis and Medical Information” section will need to be completed with the following data:
- Medication requested
- Strength and route of administration
- Frequency
- New prescription or date therapy was initiated
- Expected length of therapy
- Quantity
- Height of enrollee
- Weight of enrollee
- Drug allergies of enrolee
- Diagnosis
Under “Rationale for Request” select the applicable option. If the rationale is not present, select “Other” and provide explanation.
Step 9 – Once the document has been completely filled out and double checked for any errors, you may print it off, provide all necessary signatures, and send the document to Wellcare via Fax for processing.