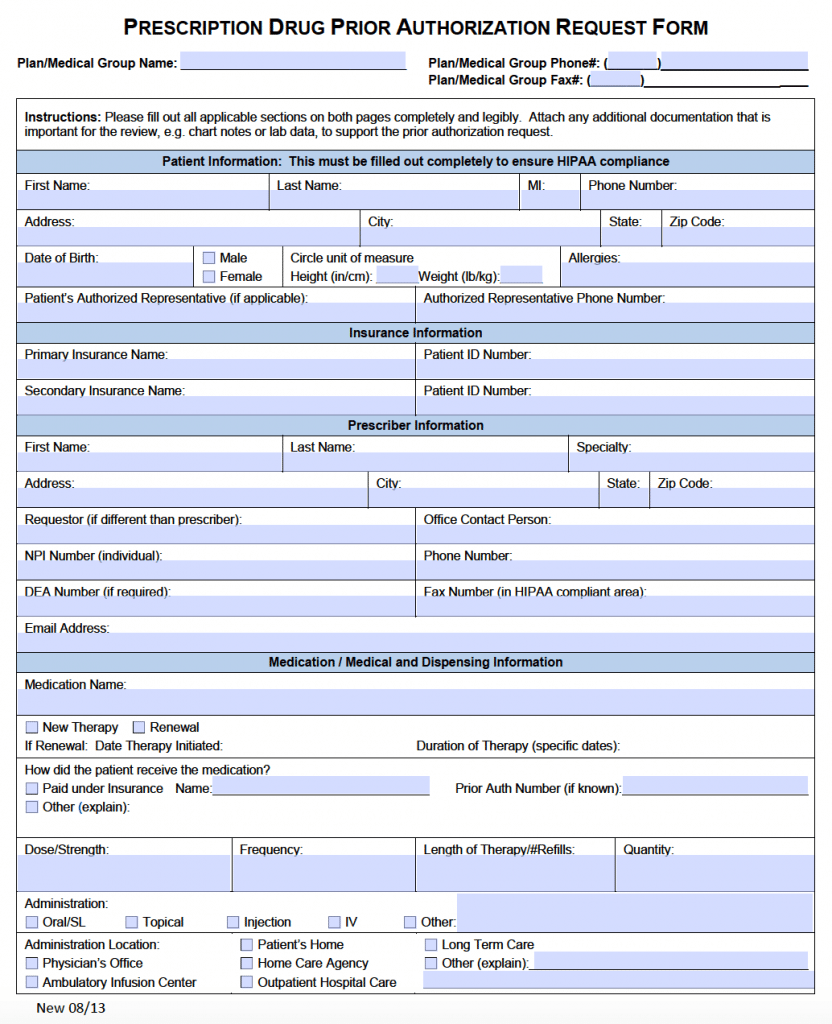
The prior prescription authorization forms are used by a doctor’s office to make a request to an insurer or government office if a drug is covered by the patient’s health insurance. The form should list the patient’s name, types of symptoms, and the reason for the drug’s medication over other approved types. After the form is complete it can be emailed or faxed and usually an answer is given between 10 and 14 business days.
Standard Prior (Rx) Prescription Authorization Form – Adobe PDF (Fillable)
Important Note: The medical office of the patient is the party required for filling-in this form, not the patient.
Table of Contents
- When to Use
- Forms by Type
- How to Write (Fill-in)
When to Use
Forms by Type
- AETNA Prior Authorization Form
- Anthem Blue Cross / Blue Shield Prior Authorization Form
- Amerigroup Prior Authorization Form
- CIGNA Prior Authorization Form
- CVS (CareMark) Prior Authorization Form
- EnvisionRX Prior Authorization Form
- Express Scripts Prior Authorization Form
- Future Scripts Prior Authorization Form
- Emblem Health Prior Authorization Form
- Express Scripts Prior Authorization Form
- Humana Prior Authorization Form
- Medicaid Prior Authorization Form
- Medicare Prior Authorization Form
- Meridian Prior Authorization Form
- OptumRX Prior Authorization Form
- PerformRX Prior Authorization Form
- Prime Therapeutics Prior Authorization Form
- Providence Prior Authorization Form
- SilverScript Prior Authorization Form
- Tufts Prior Authorization Form
- United Healthcare Prior Authorization Form
- WellCare Prior Authorization Form
How to Write
Step 1 – Download the form in Adobe PDF (.pdf).