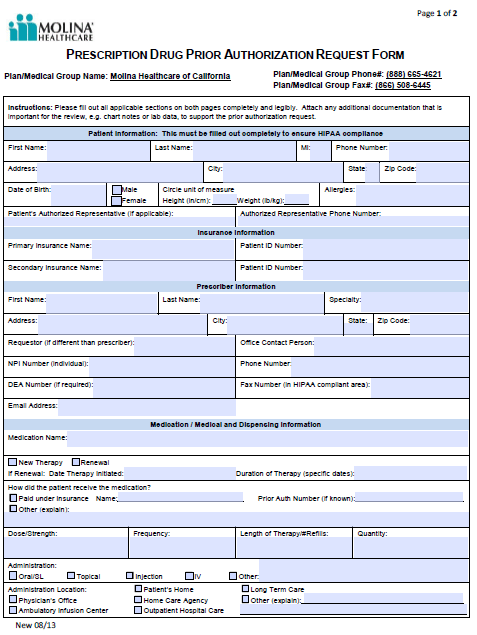
A Molina Healthcare Prior Prescription (Rx) Authorization Form can be used to request coverage for drugs that Molina Healthcare requires justification for prescribing. Along with the patient and prescriber information, the healthcare professional requesting the drug will need to specify their reasoning for doing so, including a list of diagnoses, other medication used in attempt to treat the diagnoses, and all relevant clinical information to support their claim. Each form should be completed in full, double-checked for accuracy and faxed to the number found at the top of the form.
How to Write
Step 1 – Download the state-specific form above. For the purposes of our instructions, we’ll cover the California Prescription Drug Prior Authorization Request form.
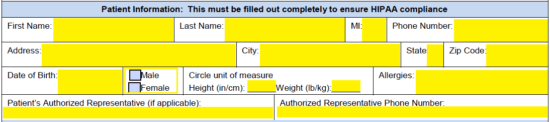
Step 2 – The patient’s personal and medical information will be required first. This will include the following:
- Name
- Phone number
- Address
- DOB
- Sex
- Height
- Weight
- Allergies
- Authorized representative (if applicable)
- Authorized representative number
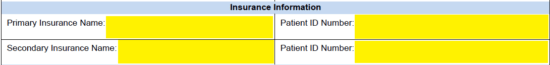
Step 3 – The name of the patient’s primary insurance and the associated patient ID number should be provided. If applicable, provide the same for the secondary insurance.
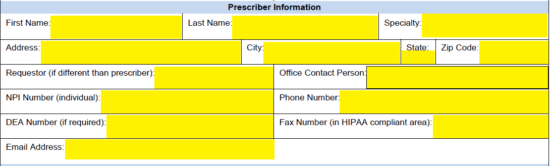
Step 4 – The presciber’s info is next. After their full name, specialty, and address have been provided, enter the following:
- Requestor (if different than prescriber)
- Office contact person
- NPI number
- Phone number
- DEA number
- Fax number
- Email address
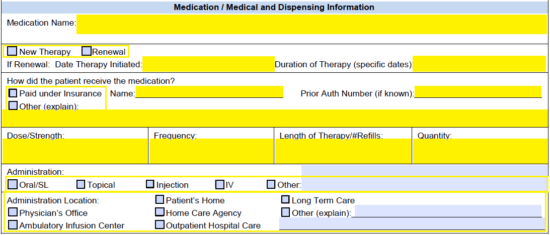
Step 5 – The name of the requested medication must be supplied here. Next, check whether this is a new therapy or renewal. If renewal provide date therapy initiated and the duration of the therapy. In the window below this, enter how the patient received the medication (paid under insurance or other) and enter the name and prior authorization if it was paid for under insurance. The requested dose/strength, frequency, length of therapy and quantity must be entered in as well. Finally check the applicable box in the administration and administration location windows.
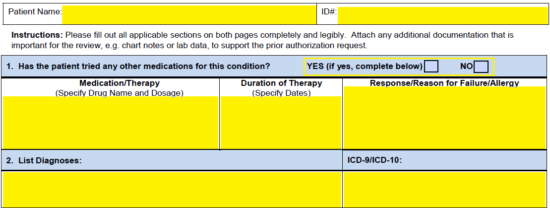
Step 6 – At the top of the second page, supply the patient name and ID#. Next, check “Yes” or “No” answering whether or not the patient has tried other medication for their condition. If yes, fill out the table the requires the medication/therapy name, the duration of said therapy, and the reason for failure. List next the diagnoses and provide the ICD-9/ICD-10 for each.
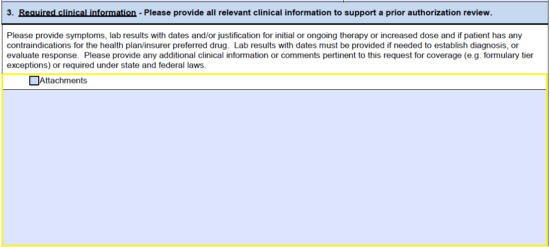
Step 7 – In the third window of the second page, provide all relevant clinical information to support the PA claim, attaching any applicable documents.
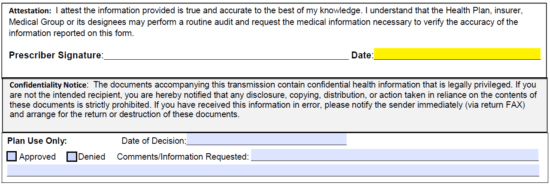
Step 8 – Enter the date of completing the form, print off the document, sign it, then send it into Molina Healthcare for review.