The CIGNA Prior Authorization Form is a simple, one-page document that allows healthcare providers to request coverage for atypical medication or those that would require coverage determination. The prescriber’s rationale for seeking prior authorization for the non-formulary request must be provided in order to justify their decision. Often forms of this nature are most effective when the alternative, formulary medication that was administered to the patient was ineffective or cause adverse effects.
CIGNA Healthcare’s coverage positions
How to Write
Step 1 – Open up the form on your web browser or download it in PDF and complete it using the PDF reader of your choosing.
Step 2 – The first window requires that you submit the provider’s info (listed below).
- Provider name
- Specialty
- DEA or TIN
- Office contact person
- Office phone and fax
- Whether fax machine is kept in secure location
- Whether CIGNA can fax the response to the office
- Office address

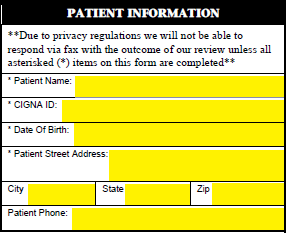
Step 3 – The required patient’s information includes their name, CIGNA ID, date of birth, address, and phone number.
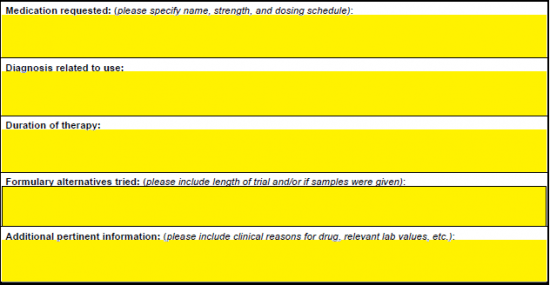
Step 4 – Here is where the requested information must be detailed. Enter the name, strength and dosing schedule of the medication in the first window. Next, supply the patient’s diagnosis related to use. In the third (3rd) window, the duration of therapy can be explained. The bottom two (2) fields are for the justification for prescribing the medication. First supply the formulary alternatives that were attempted, then supply whatever additional information is applicable and pertinent (e.g. clinical reasons, relevant lab values).
Step 5 – Fax the completed form to 1 (800) 390-9745 after it has been double-checked for accuracy.

