The Cigna-Healthspring Coverage Determination Form is available to those healthcare practitioners wishing to provide their patients with the best possible treatment at the most affordable prices. Cigna-Healthspring specializes in assisting Medicare and Medicaid beneficiaries, and it is those patients who are covered under their Medicare Part D Prescription Drug Plan that will be able to employ the attached form. The coverage determination form is a blanket document that encompasses a variety of purposes, prior authorization being one of them. Those wishing to receive coverage for a drug which is non-formulary or atypical will need to have the prescriber provide justification for the selection of said drug.
How to Write
Step 1 – Download the fillable form in Adobe PDF and open it up on the PDF reader of your choice.
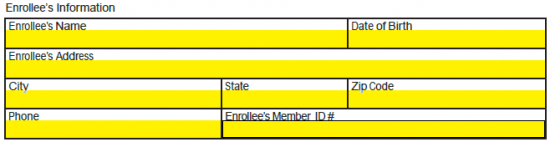
Step 2 – Once the form is open in your computer, enter in the “Enrollee’s Information.” The following data will be required:
- Full name
- Date of birth
- Full address
- Phone number
- Member ID
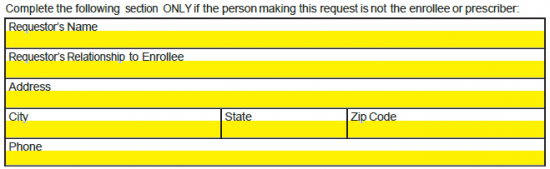
Step 3 – If the requestor is not the enrollee nor the prescriber, they must also provide their personal information. This will include their full name, relationship to the enrollee, address, and phone number.
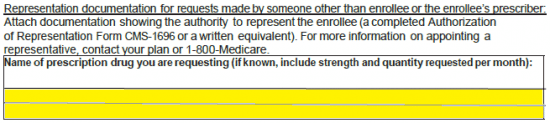
Step 4 – If a representative of the enrollee, ensure that you attach an authorization form equivalent to Form CMS- 1696. Next, provide the name of the requested prescription drug and, if known, the strength and quantity.
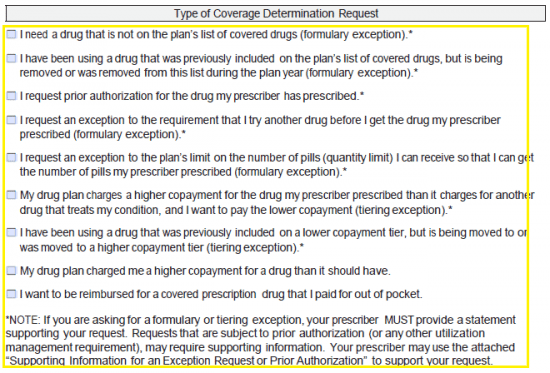
Step 5 – Under the “Type of Coverage Determination Request” window, select the “I request prior authorization for the drug my prescriber has prescribed” checkbox.
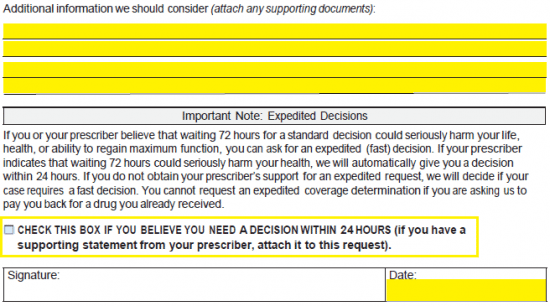
Step 6 – If additional information should be taken into consideration, supply this info in the empty fields at this juncture. If you need Cigna-Healthspring to make a decision within twenty-four (24) hours, check the box under the note explaining expedited documents. Provide the date and, once the document is printed, your handwritten signature.
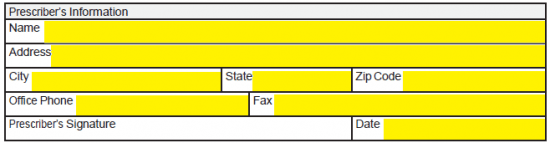
Step 7 – This section of the form is designated for those requesting prior authorization. The prescriber’s info will be needed first including their name, address, office phone and fax, the date, and their signature.
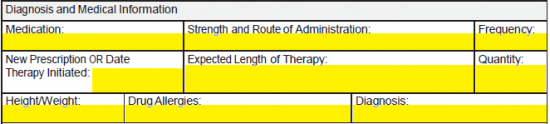
Step 8 – Diagnosis and medical information must be entered into this window. Provide the following:
- Medication
- Strength and route of administration
- Frequency
- New prescription or date therapy initiated
- Expected length of therapy
- Quantity
- Height/Weight of patient
- Drug allergies
- Diagnosis
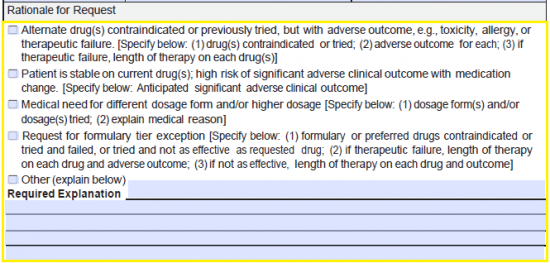
Step 9 – The rationale for the request must be selected from the five (5) options. If the first four (4) do not apply, check the fifth box and provide your explanation.
Step 10 – Once the form has been printed, supply the appropriate signatures of the prescriber, enrollee, and requestor (if applicable). Fax the form to 1 (866) 845-7267, or mail it to:
Cigna-HealthSpring Pharmacy Service Center
Attn: Part D Coverage Determinations and Exceptions
PO Box 20002
Nashville, TN 37202