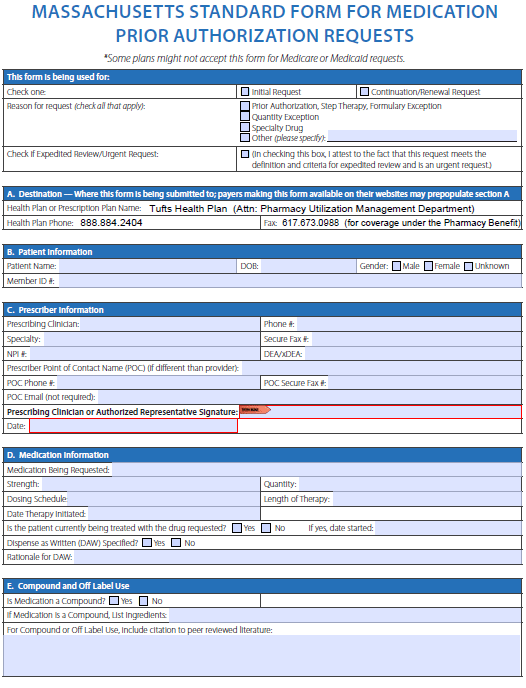
TUFTS’ Prior Authorization Form can be used by healthcare professionals in Massachusetts and New Hampshire to request coverage for a drug not on the insurance company’s drug formulary. Drugs that require prior authorization are generally those which are specialized, unconventional, or more expensive. This thorough document allows for the healthcare provider to supply ample reasoning for their request which in turn provides the insurance company with sufficient information to make an informed decision.
How to Write
Step 1 – Download the state-specific form above to begin the request process. Once open on your computer, proceed to the next step.
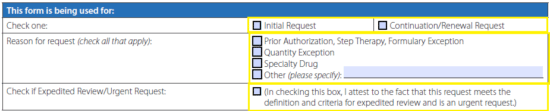
Step 2 – Select either “Initial Request” or “Continuation/Renewal Request” to start. Below that, select the reason for the request (in this case prior authorization) and, if this is an “urgent request,” check the applicable box.
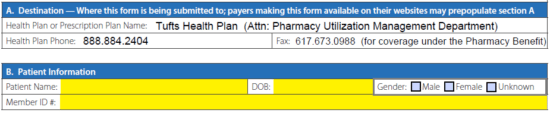
Step 3 – Under “Patient Information,” supply their name, date of birth, gender, and member number.
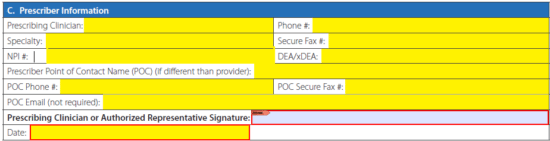
Step 4 – The prescriber information is slightly more involved. Enter all of the following:
- Clinician’s name
- Phone number
- Specialty
- Fax number
- NPI number
- DEA/xDEA
- Prescriber contact person (if applicable)
- Contact person’s phone
- Contact person’s fax
- Contact person’s email (optional)
- Signature (once printed if filling online)
- Date
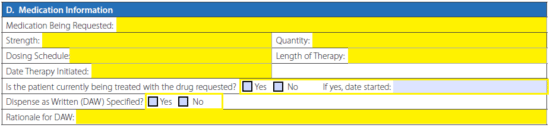
Step 5 – Window “D” asks for the information relating to the medication being requested. Supply the name, strength, dosing schedule, quantity, therapy length, and date therapy is initiated. If the patient is currently being treated with the request drug, check the appropriate box and provide the start date. Check “Yes” or “No” when asked if the DAW is specified and, if “Yes,” supply your rationale
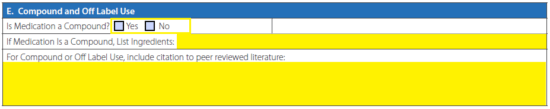
Step 6 – Answer whether or not the medication is a compound and, if it is, provide a list of its ingredients. Include citation to peer reviewed literature if applicable.
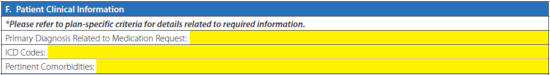
Step 7 – In section “F” you can enter the primary diagnosis related to the request, the accompanying ICD codes, and pertinent comorbidities.
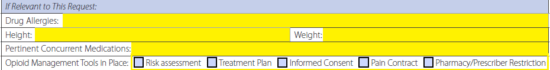
Step 8 – In this section, the following can be provided:
- Drug allergies
- Member height
- Member weight
- Concurrent medications
- Opioid management tools in place (if applicable)
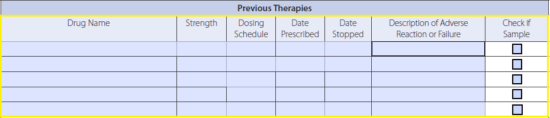
Step 9 – List the details relating to each previously attempted therapy for the patient’s diagnosis.
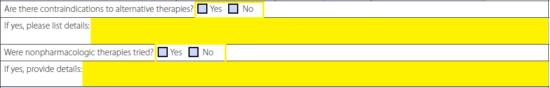
Step 10 – Check the appropriate checkbox for each of these questions. If the answer is “Yes” to either, provide the requisite details.
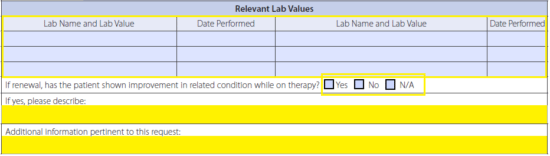
Step 11 – Under “Relevant Lab Values,” if applicable, provide lab name and value and the date of each test. If the request is for a renewal, check the appropriate box relating to any improvement while on the therapy. If the answer is “Yes,” describe. Any additional information for the request can be provided in the bottom field here.
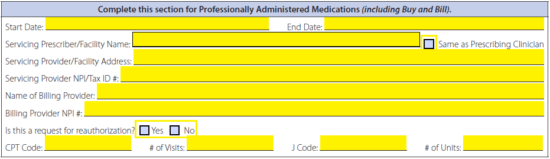
Step 12 – This window is to be completed for “Professionally Administered Medications”. Supply all requisite information if this applies.
Step 13 – Once all data has been entered into the form, you can print it off, provide the aforementioned signature, and fax it with any other supporting documents to (617) 673-0988.