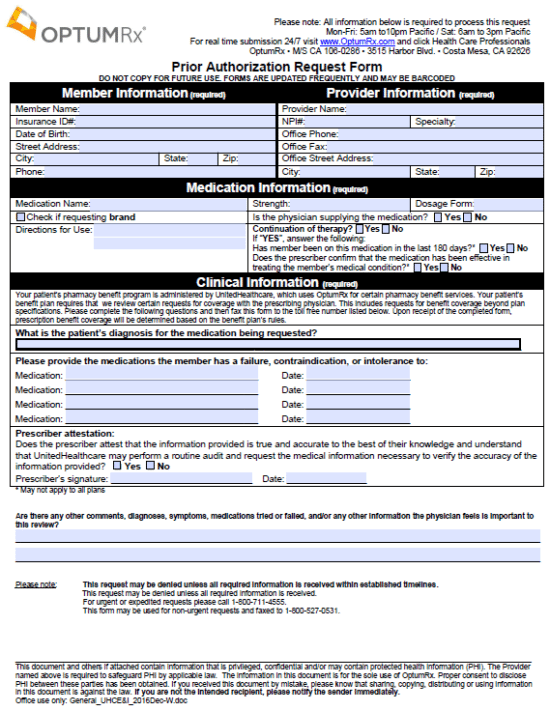
The OptumRX Prior Authorization Request Form is a simple form to be filled out by the prescriber that requests that a certain treatment or medication be covered for a patient. A list of tried and failed medication must be provided as a justification for the request alongside the diagnosis. This info will allow those at OptumRX to determine whether or not partial or full coverage is feasible. This form must be completed in full and double checked for accuracy before being faxed to the insurance company for review.
How to Write
Step 1 – Begin by downloading the form in Adobe PDF and opening it up in the PDF reader of your choice.
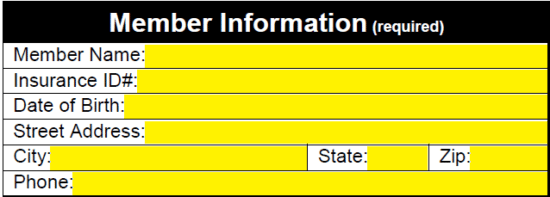
Step 2 – The first required information is that of the member. Enter their name, insurance ID number, DOB, full address, and phone number.
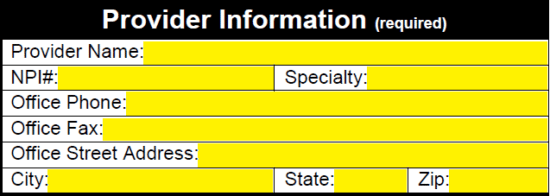
Step 3 – Next, to the right of the member info, supply the healthcare provider info. This will require the following:
- Name
- NPI #
- Specialty
- Office phone
- Office fax
- Office address
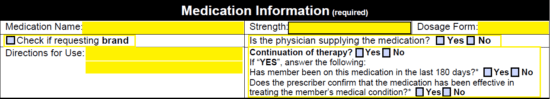
Step 4 – The medication’s name, strength and dosage form must be enter next. If requesting a brand, select the appropriate box. If the physician is supply the medication, check that this is the case. In the two bottom windows, enter in the directions for use and whether or not it is a continuation of a current therapy. If yes, answer the two accompanying questions.
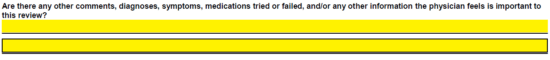
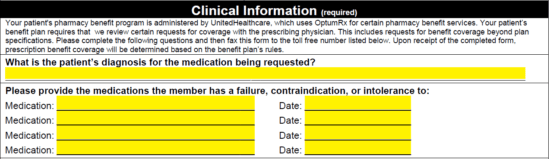
Step 5 – The clinical information window is required. Supply the diagnosis followed by a list of medications that have been tried and failed and the date on which each drug was prescribed.
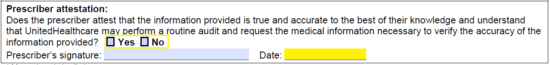
Step 6 – Check the “yes” box to indicate that all the information provided is both true and accurate. Enter in the date and, once the document has been printed off, sign the signature field. Before doing so however, enter in any other comments, diagnoses, symptoms etc. that will help the reviewing process.
Fax the form, once 100% complete, to 1 (800) 711-4555 if this is an expedited request, or to 1 (800) 527-0531 if the need for the medication could be classified as non-urgent.