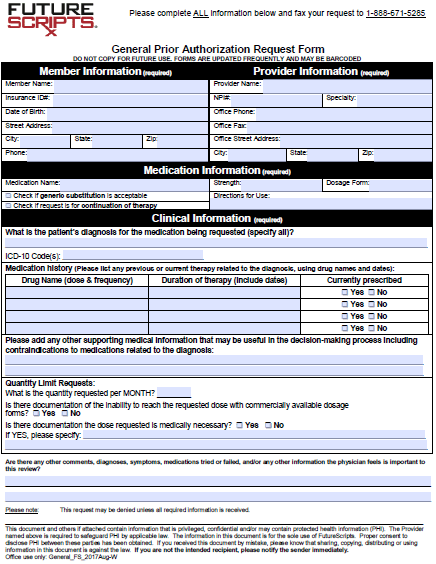
The Future Scripts General Prior Authorization Request Form is a document that can be faxed into Future Scripts to request coverage for a medication which is generally not on the company’s formulary. The prescriber will need to provide justification for selecting the medication in question to treat the patient’s symptoms. Often previous drugs and treatments have been applied prior to administering this form; each one should be detailed within the form to strengthen the case for coverage.
How to Write
Step 1 – Begin by downloading the Prior Authorization Form.
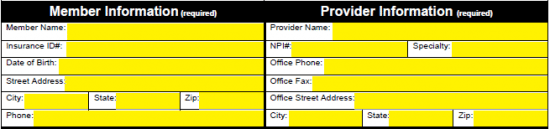
Step 2 – With the form open on your computer, you can begin to fill in the requisite info. Under “Member Information” you can submit their full name, insurance ID number, DOB, full address, and phone number. The following information pertaining to the healthcare provider will need to be submitted in the window on the right:
- Provider name
- NPI#
- Specialty
- Office phone
- Office fax
- Full office address
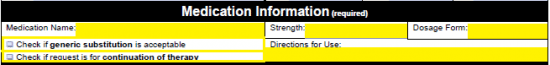
Step 3 – Enter the medication name, the strength, the dosage form and the directions for use. There are two checkboxes in the “Medication Information” window as well, one if generic substitution is considered acceptable and another if the request is for a continuation of an already active therapy.
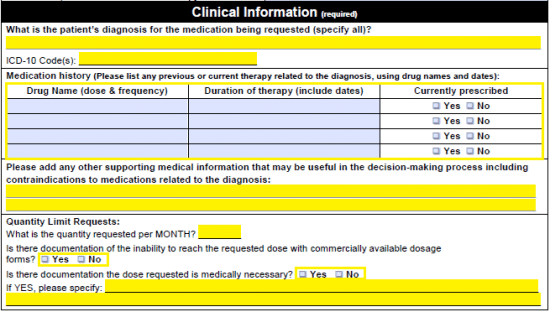
Step 4 – In the top field under “Clinical Information,” supply the patient’s diagnosis. The ICD-10 Code(s) should be submitted immediately under. Each dosage, frequency, and duration of each previously prescribed therapy should be indicated in the table. You must also answer whether or not the individual is still prescribed to the medication in question. You will also need to to add any other supporting medical information that could be useful for coverage determination.
The following questions must be answered as well before proceeding:
- What is the quantity requested per month?
- Is there documentation of the inability to reach the requested dose with commercially available dosage forms?
- Is there documentation that states that the dose requested is medically necessary? (If yes, specify)
Step 5 – Any other comments deemed pertinent to the prior authorization request can be submitted before printing the document and sending it to: 1-888-671-5285.