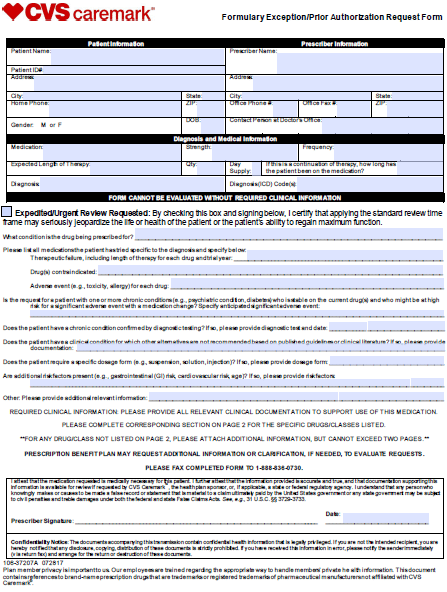
The CVS Caremark Prior Authorization Request Form can be used to request coverage for a non-formulary medication or one which is more expensive than those which are typically covered by the insurance company. The below form must be completed in its entirety by the medical practitioner prescribing the drug. The healthcare professional must supply the member and prescriber information as well as the justification for prescribing the non-formulary treatment. Furthermore, all relevant clinical documentation must be attached to provide reasoning for the selection of the medication in question.
How to Write
Step 1 – Begin by downloading the CVS Caremark Prior Authorization Form.
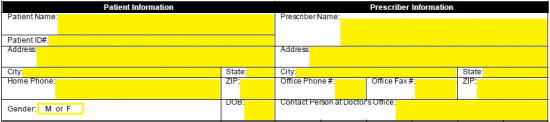
Step 2 – The first two windows require the patient and prescriber information. For the patient, provide the following:
- Full name
- Patient ID#
- Full address
- Home phone
- Gender
- Date of birth
Enter the below prescriber info:
- Full name
- Full address
- Office phone number
- Office fax number
- Contact person at office
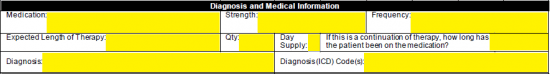
Step 3 – The suggested medication, strength and frequency must be supplied in the window pictured below. Also, the expected length of therapy, quantity and day supply must be supplied. If this is a continuation of a previous therapy, enter in how long the patient has been on the medication. Finally, the diagnosis and diagnosis codes can be specified.
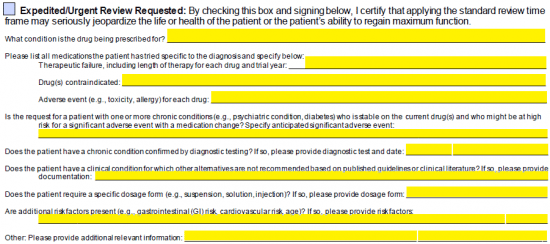
Step 4 – If the review of the form should be expedited, check the applicable box. Answer all medical related questions below to give full reasoning for prescribing the specific drug.
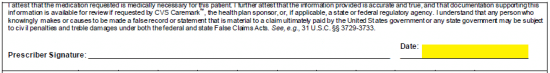
Step 5 – Provide the date of the request next to your signature once the document has been printed off.
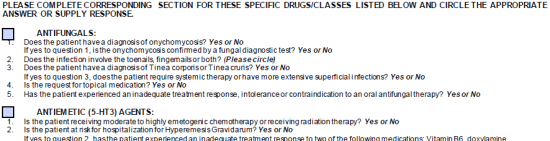
Step 6 – Check the applicable box for the specific class of drugs if necessary. Under the checked box, circle “Yes” or “No” to the questions posed.