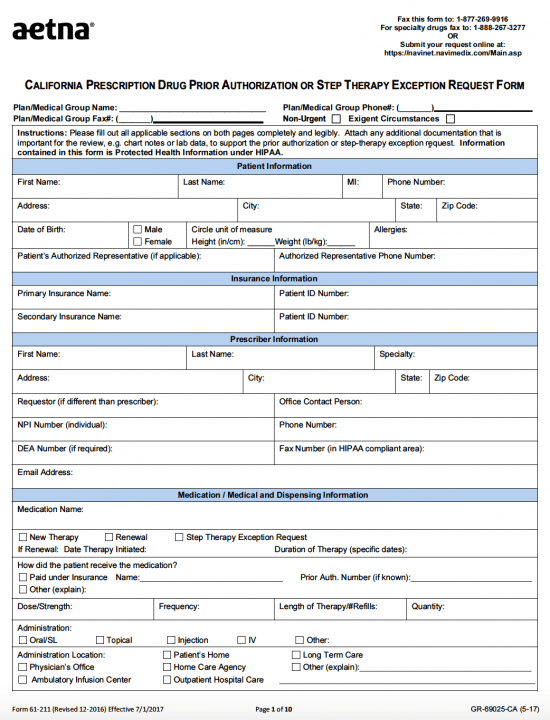
The AETNA prescription prior authorization form is a document that is used to justify the prescribing of a particular medication not already on the AETNA formulary. The patient’s personal insurance information, their current condition, and the previous drugs/therapies attempted to remedy their condition must be supplied. If prior authorization has been granted, the insurance company will pay for either a part or the entire cost of the prescribed medication. We’ve linked all state-specific forms below for your convenience and have included a run through of the form to ensure that all information supplied is accurate.
Types
How to Write
Step 1 – Download the .zip file with all the forms or one (1) of the following States:
Step 2 – This example will be only for the State of California but can be applied generically to all other forms.
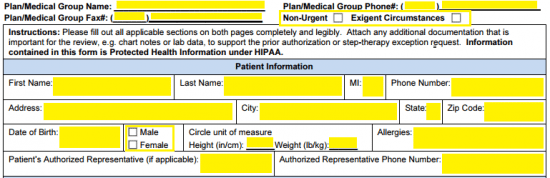
Step 3 – The first emboldened fields at the top of the form will require the Plan/Medical group name, and the group phone and fax number. After selecting whether the situation could be described as “Non-Urgent” or “Exigent Circumstances,” provide the following, standard patient information:
- Full name
- Phone number
- Full address
- Date of birth
- Gender
- Height
- Weight
- Allergies
- Patient’s authorized representative (if applicable)
- Representative phone number
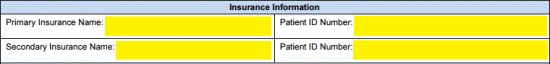
Step 4 – The patient’s insurance information will be required next. Supply their primary and secondary insurance names and the corresponding ID numbers.
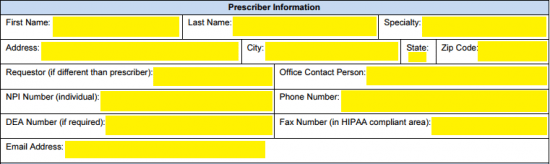
Step 5 – Now for the prescriber information. This will require that the below data be entered into the appropriate fields.
- Full name
- Specialty
- Full address
- Requestor
- Office contact person
- NPI number
- Phone number
- DEA number (if necessary)
- Fax number
- Email address
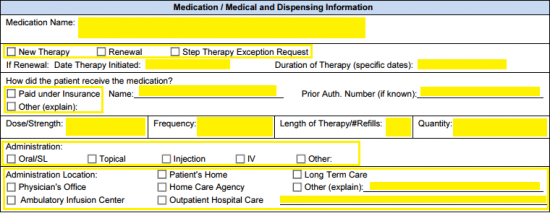
Step 6 – Details surrounding the medication and the dispensing of said medication are to be entered in here. After the name has been submitted in the top-most field, the following must be supplied:
- Whether new therapy, renewal, or step therapy exception request
- If renewal, the date the therapy was initiated and duration of therapy
- How patient has received medication (paid under insurance or other)
- If paid under insurance, enter the name and prior authorization number
- If other, provide an explanation
- Dosage/Strength
- Frequency
- Length of Therapy/number of refills
- Quantity
- Administration
- Administration location
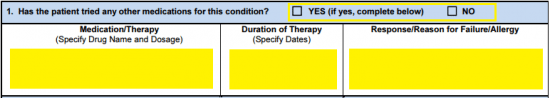
Step 7 – On the second page, start off by answering whether the patient had tried any other medications for the condition. If so, specify the drug name and dosage, the duration of the therapy, and the reason for failure.
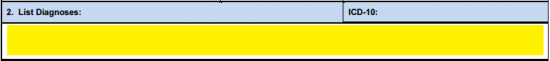
Step 8 – List the diagnoses and the ICD-10 classification.
Step 9 – All relevant clinical information that can be used to support the argument for prior authorization should be submitted in the large space in field three (3). If attachments are necessary, check the box that indicates that this is the case.
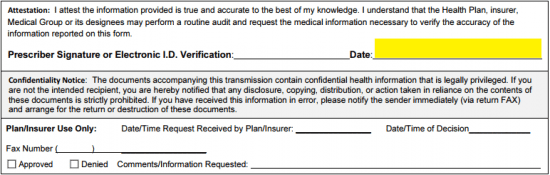
Step 10 – Supply the date in the applicable field, read the attestation statement, double check the form and provide your signature. Send the completed document to AETNA via fax at: 1 (877) 269-9917.