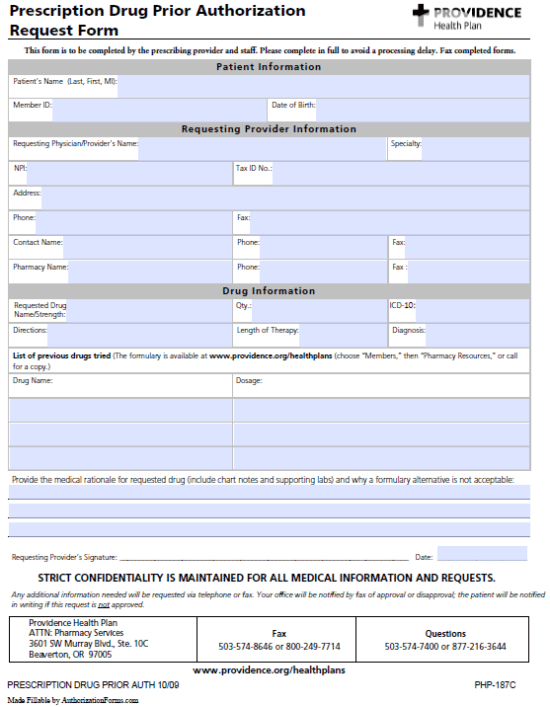
The Providence Prescription Drug Prior Authorization Request Form is a document that is used to acquire coverage for prescription medication which requires authorization, that is, drugs that are not automatically covered by the member’s health plan. Prescribers or other authorized representatives will be required to complete the document in full, providing their medical rationale for suggesting this particular medication over other formulary alternatives and listing all previously attempted solutions to the patient’s diagnosis. Once the form has been completed, it can be faxed to: 1 (503) 574-8646 or 1 (800) 249-7714.
How to Write
Step 1 – First you’ll have to download the form. Click here and open up the document in your web browser or PDF viewer of choice.
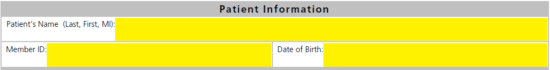
Step 2 – The first info you’ll need is the patient’s name, member ID and DOB.
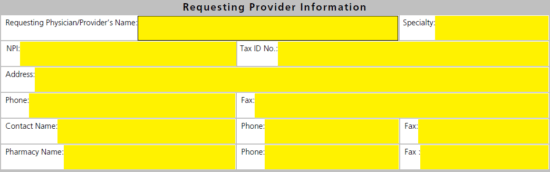
Step 3 – Here you can supply all the medical provider’s info. Submit the following:
- Requesting physician/provider’s name
- Specialty
- NPI
- Tax ID #
- Full address
- Phone number
- Fax number
- Contact name, phone, and fax
- Pharmacy name, phone, and fax
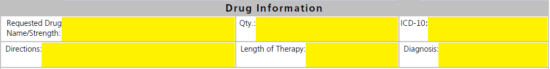
Step 4 – Request drug name and strength must be submitted into the first field followed immediately by the quantity and ICD-10. On the second line, enter in the directions, length of therapy and diagnosis.
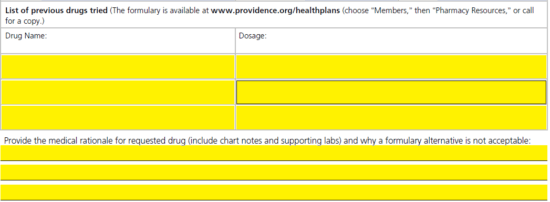
Step 5 – Here is where the reasoning for prescribing the chosen medication must be justified. Provide a list of previously drugs tried and the dosage of each. Below the table, in paragraph format, supply your medical rationale for the request drug all with any supporting chart and labs notes (attach as separate pages if necessary).
Step 6 – Print off the form once double checked for accuracy, supply the day’s date and your signature then fax the document and any other necessary information to 1 (503) 574-8646 or 1 (800) 249-7714.