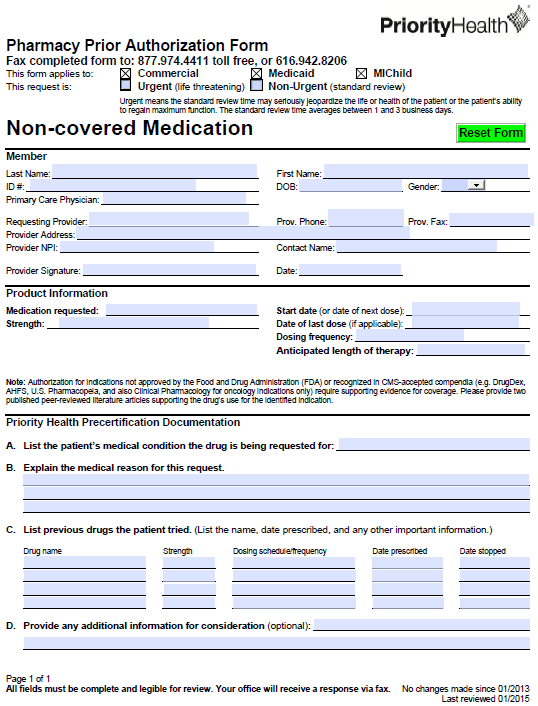
A PriorityHealth Pharmacy Prior Authorization Form is a way for plan members to receive coverage for non-covered medication. This form should be completed by the prescriber or healthcare professional in order to provide sufficient justification for the necessity of the non-formulary to treat their patient’s current diagnosis. The below form can be used for commercial, medicaid and MIChild insurance. Once completed, fax to 1 (877) 974-4411 or 1 (616) 942-8206.
How to Write
Step 1 – Download the form in Adobe PDF to begin.
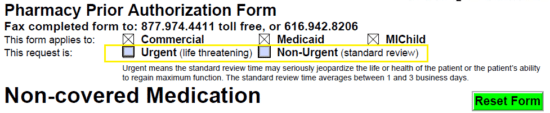
Step 2 – Once the form is open on your computer, check whether or not the request is urgent or non-urgent.
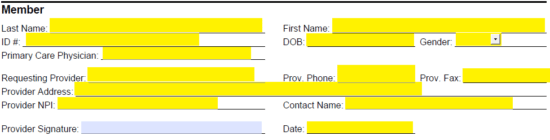
Step 3 – The first window requests the member’s full name, ID #, date of birth, gender, and physician’s name. Next supply the following info pertaining to the provider:
- Provider name
- Phone number
- Fax number
- Address
- NPI
- Contact name
Once the form has been printed off, the date of signing and the signature can be supplied.
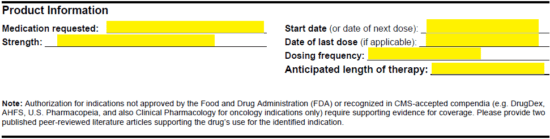
Step 4 – Here the product information can be supplied. This will require all of the below data.
- Medication request
- Start date
- Strength of medication
- Date of last dose (if applicable)
- Dosing frequency
- Anticipated length of therapy
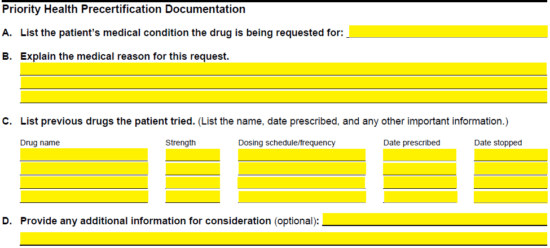
Step 5 – Here is where the medical reasoning for the non-covered medication can be supplied. List the patient’s medical condition and explain the medical reasoning in paragraph format. A full list of previously attempted drugs to treat the conditions should be supplied and below that, any additional information that may support the argument.
Step 6 – Print off the form, provide the provider signature as mentioned in step 3, then fax the completed form to the numbers found at the top of the page.