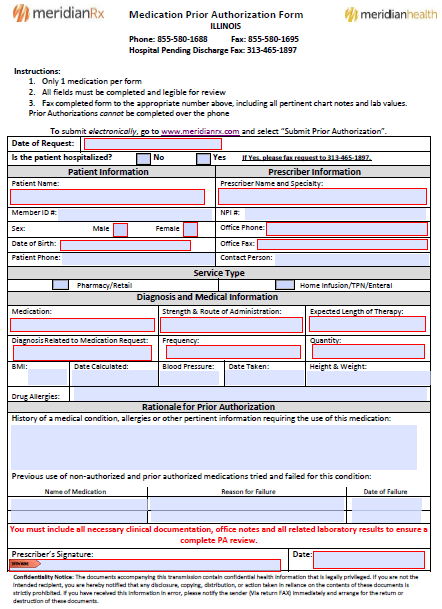
The Meridian Medication Prior Authorization Form is one that can be used to request coverage for a prescription medication. An authorization request of this variety will need to be completed by the healthcare provider and sent either online through the Meridian Prior Authorization website or via fax using the state-specific forms linked on this webpage. Alternative medication is usually granted coverage providing that formulary medication has been attempted prior to the submission of a prior authorization form. Evidence of previously attempted treatments will often strengthen the case of the requester.
How to Write
Step 1 – Begin by downloading the form in Adobe PDF (Illinois, Michigan).
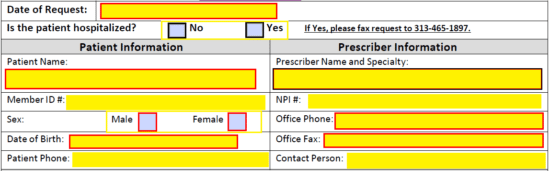
Step 2 – The first portion of the form requires that you provide the date of request and answer whether or not the patient is hospitalized. Under “Patient Information”, enter their name, member ID#, sex, DOB, and phone number. The following prescriber info will be required on the right:
- Prescriber name and specialty
- NPI #
- Office phone
- Office fax
- Contact person
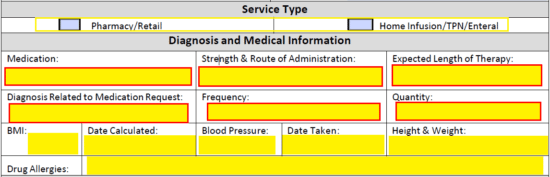
Step 3 – Specify here the service type. Next, relay the diagnosis and medication information. This will require the below data.
- Medication
- Strength & route of administration
- Length of therapy (expected)
- Diagnosis related to request
- Frequency
- Quantity
- BMI
- Date calculated
- Blood pressure
- Date taken
- Height and weight
- Allergies
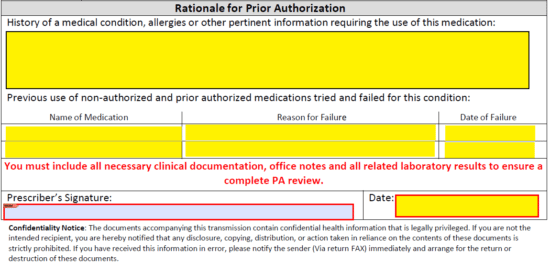
Step 4 – The large paragraph field at this juncture should be used to provide all information that leads to the use of the requested medication. Provide allergies, medical condition, and any other data that may support your case. List previous used non-authorized and prior authorized medications in the table below the field.
Provide the date, then supply your signature before faxing the completed form to (855) 580-1695 if in Illinois or (877) 355-8070 if in Michigan.